NB – if unsure, ALWAYS consult with your Stoma Nurse and never assume anything, these are just general guidelines. Your specific medical history, stoma, and needs should be taking into consideration as some information is case specific and does not apply to all.
When it comes to dieting you always must eat a well-balanced diet to keep your body in optimum condition and especially after surgery to rebuild your strength. When you become an ostomate you must realize that your GUT has been shortened and you must make a few slight changes to the way you eat, meaning you have to chew your food a lot more to assist in the digestive processes, eat slower and if needed smaller meals more frequently, and always have an adequate fluid intake. It is important to speak to your dietician when you have any chronic diseases like Diabetes, Renal Failure, Hypertension, etc., as these conditions will require special diets that needs to be adjusted for your specific medical condition and needs.
Thus, after consultation with your physician and dietitian about your specific medical condition and diet, there are a few general guidelines that might be followed when it comes to your diet, but before we discuss this, you need to first identify which type of stoma you might have because as we are all different, with different chronic illnesses and different stoma’s, there is not one specific diet that will work for all. In the beginning it is best to keep a diary and check how your body and stool output reacts to the various foods you eat, so that you can become aware of what works for you and what not.
Taste: After your surgery you might find that your food does not taste the same as it did before, or most patients verbalize that they have a “steel” like taste in their mouths, or that the food they used to love they now cannot stand, etc. This is all normal and will over time settle, what is however most important is that you must eat food. If you cannot eat a full meal, please divide the meals into smaller meals more frequently during the day, but you must get all the nutrients into your body that is needed to gain your strength and assist you on your road to recovery.
Medication: It is important to continue taking your chronic medication as prescribed by your physician and any other medication given after discharge from hospital. Medication can influence your stool output, for example it can change the color, cause either constipation or diarrhea, etc., therefore it is vital that you speak to your pharmacist when you collect your medication if you have any concerns or uncertainties.
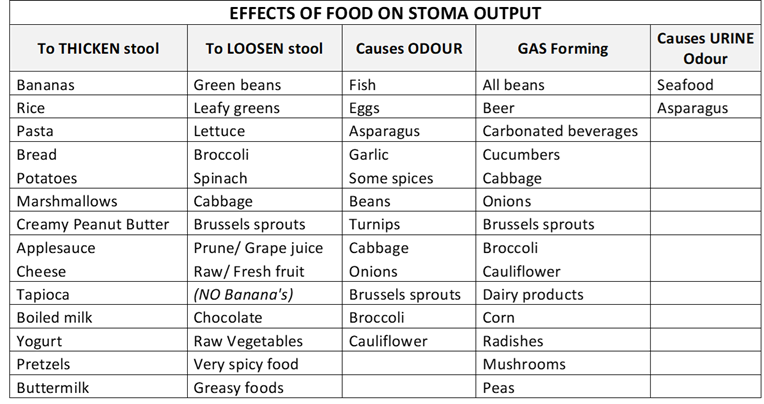
Colostomy: Most colostomies are situated on the left side of the abdomen but could be situated on various places on the abdomen depending on where in the large intestine the diversion needed to be made due to various medical conditions which might have required the formation of this stoma. What is variable here is that the closer the stoma is to the anus, the thicker the stool will be due to the amount of water absorbed as the stool passed through the large intestine. A colostomate therefore must know where their stoma is in the large intestine in order to ensure that they can manage the correct consistency of stool output. As a general rule, lower on the left side the colostomy normal output should be the consistency of toothpaste, anything else is either constipation or diarrhea for this specific stoma. Therefore, please speak to your Stoma Nurse and ensure that you are aware of what a normal stool should be like for your specific colostomy in order to manage your diet accordingly, and as per prescription of your dietician and physician with regards to chronic diseases. Below find a list of suggestions to manage your output when either too soft or too hard with food before you take medications.
Always speak to your support team of multidisciplinary experts if unsure and before you make major changes to your new lifestyle, but always remember to enjoy every new and additional day you were granted.